I’m 42, Newly Diagnosed With Type 1 Diabetes…And I’m FREAKING OUT!
Getting Diagnosed With Type 1 Diabetes As An Adult
What a long, strange trip it’s been. Well, not really. Actually, I was just diagnosed with diabetes about a month ago as of this writing. So it’s been a relatively short trip. But the mental, emotional, and physical rollercoaster I’ve been on since I was diagnosed with diabetes makes it feel much longer. Add to it all the fact that a couple of weeks in I was actually diagnosed type 1, and things really got dicey.
This is a quick look at what I’m now calling my “four stages of starting to get my sh*t back together after being diagnosed with diabetes.”
Things I see in hindsight now, but hopefully you or a loved one will be able to use from day one. More on my extremely aggressive type 1 diabetes symptoms in the weeks leading up to my being diagnosed with diabetes later. We’ll start with getting the news.
Sign Up Now For New Travel Tips & Inspiration
This site participates in the Amazon Services LLC Associates Program and other affiliate programs and may earn from qualifying purchases.
DISCLAIMER: Always consult a healthcare professional before making any medical decisions. The information on this website should not be used as a substitute for professional medical care or advice. It provides general information and does not make any warranties about the completeness, reliability, or accuracy of this information. Type 1 diabetes travel will not be liable for any losses and/or damages in connection with the use of this website.
Week 1 – Leading Up And Then Getting The News
It’s interesting. The weeks leading up to my diagnosis were clearly tracking towards diabetes. I had recently researched all the diabetes symptoms I was having ((blurry vision, drinking tons of fluids, excessive urination, crankiness, exhaustion, crazy weight loss…), and it just seemed clear as day.
Did you know: High blood sugar can make the lenses of your eyes swell, temporarily blurring vision.
Getting blood sugar back in range—typically 70-130 mg/dL before meals and under 180 mg/dL after eating—usually clears it up. Wish I had known that before I spent about $500 between eye doctors and two new pairs of glasses the weeks before my type 1 diagnosis. But I digress.
But I was hunkering down with friends in Michigan for a couple of months and didn’t have a doctor up there. I made an appointment for the day I would get back to my sometimes home base back in North Carolina and would go from there.
I understood the symptoms of diabetes that I was having, and had kind of resided myself to the reality that it would be confirmed. It was almost as if I was at peace with the reality. I kind of had some weird “welp, I guess that’s that,” passive nonchalance about it as if it was no big deal and life would go on without much fanfare.
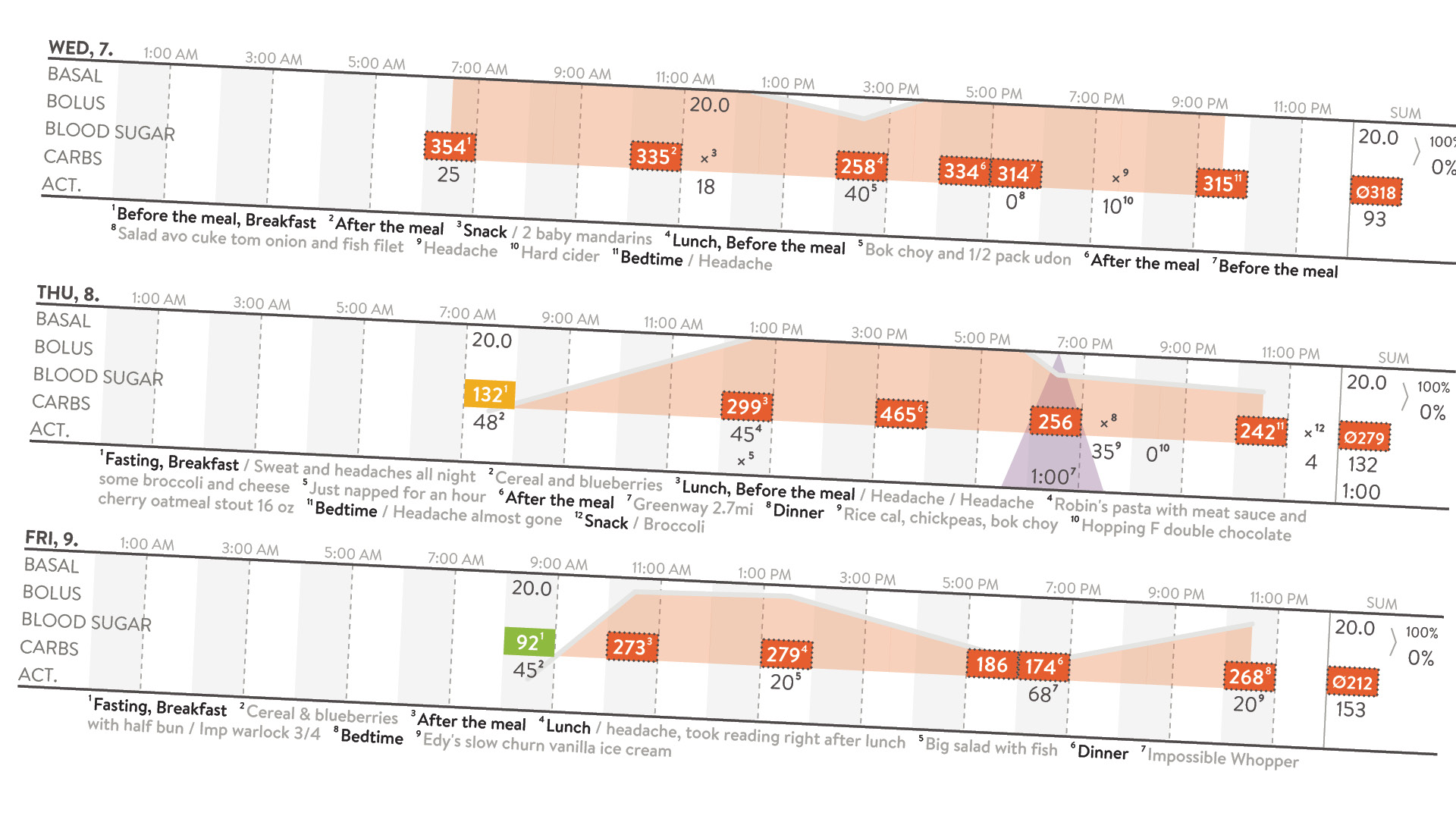
I went to my doc and dropped the knowledge about my recent changes. They took my HGB A1C and it had gone from 6.6 to almost 13 in just under 5 months. My estimated blood glucose level was 318mg/dL in that range.
What is HGB A1C you ask? It’s a Hemoglobin A1C test that shows your average blood sugar levels for the past 2 to 3 months. “Normal” is under 5.6…and mine was 12.7. And “normal” range for blood glucose is between 80-120mg/dL…and mine was averaging above the 320s.
That’s When I Was “Officially” Diagnosed With Diabetes
Well, type 2 diabetes, but we’ll get to that later. The words “you have diabetes” were said, and my doctor spent the next 45 minutes unloading a firehose of overwhelm on me. Detailing what needed to change immediately and how this would affect me for the rest of my life.
Week 1 – Getting Shellshocked; Zombie-Mode…Engaged
Within minutes of that moment when I was “officially” diagnosed with diabetes, the doctor’s words started to sound a lot like that teacher in the old Peanuts cartoons:
“If you don’t take care of your Diabetes…Whaa….Waaaa…Whoooomm…Waaaa. Complications could be…Whaa….Waaaa…Whoooomm…Waaaa. Let’s get you on basal insulin…Whaa….Waaaa…Whoooomm…Waaaa. See you in a couple weeks!”
Now understand, I’ve spent my entire life as a fairly detailed guy. In case you haven’t been following along, I’m annoyingly analytical and an eternal devil’s advocate. I’m always looking at multiple angles. But as I sat alone with my new diagnosis, being barraged with information, I just got overwhelmed.
Then at that moment I kind of just shut down. As much as I was trying to listen and take it all in, things kind of started to turn into a hum and I couldn’t focus.
I Just Nodded, Like Incessantly…
I acknowledged what I was being told while barely grasping any of it at that actual moment. The doc sent me home with a bunch of new, expensive prescriptions for things I didn’t understand, like metformin and a basal insulin pen that I was supposed to shoot up with daily.
Honestly, the next week was spent essentially in two modes: research mode and zombie mode. I was either reading everything possible about being diagnosed with diabetes or sitting and staring into nowhere, shellshocked at the entire lot of it. I got very little actual work done otherwise, and if I did, it was likely pretty shoddy.
Week 2 – Steps Towards Proactivity & Aggressive Action
The first week after I got diagnosed with diabetes is still a little blurry, no matter how I try to recount it. But I do remember being very frustrated with my primary care physician (PCP) and the passive way she seemed to have glossed over my A1C level from my previous physical.
See, “prediabetic” A1C levels are those between 5.7 and 6.4. Mine was 6.6 at my previous physical, but the doc pretty much said “you’re in prediabetic range and you’re going to want to keep an eye on that” and sent me on my way.
Back then I definitely didn’t understand what an A1C was and I definitely didn’t understand the potential implications of actually being diagnosed with diabetes. Combine that with an extreme lack of concern from the doctor and no urgency in following up or starting treatment at all, and I ignorantly just kept business as usual. I mean, she didn’t really seem concerned, so I took her lead. Big mistake.
And yes, I’m still pissed, especially since she later stated (…in an email no less…) that she “should have requested for you to follow fairly quickly after discovery of any abnormal lab tests.” Her exact words, not mine.
But I digress.
Week 2 – My First Appointment With A Diabetes, Endocrinology & Metabolism Specialist
That was the point where I realized that I needed to see a diabetes specialist. Now, I’ve been fairly healthy my whole life and typically only go to the doc for yearly routine maintenance and my physical. I’ve been blessed to have decent insurance in the past that I rarely needed to use… or understand really. And I definitely hadn’t had to dive into the world of “specialists” or how to find or work with them.
Yes, that’s a privilege and/or luck, but regardless, it meant that I really didn’t know how to proceed. So I just started searching the interwebs for things like “diabetes specialist near me” and “diabetes specialist reviews” and went from there. A few more hours later I found some names within my network. I requested that my PCP fill out the proper referral paperwork to get me an appointment. One week after initially being diagnosed with diabetes, I was in my new endocrinologist’s office.
But this time was different. This doctor clearly had much deeper knowledge of the disease. And I had spent the past week at least getting a base understanding of diabetes, the terminology, potential care steps, etc.
Yeah, You’re Type 1…
The first thing my endo said when he walked in was “yeah, you’re type 1, but let’s run some tests to make sure.” This was mostly based on looking at my previous medical history and my physical traits, but he was right.
To confirm a type 1 diabetes diagnosis as opposed to type 2 diagnosis, an endocrinologist can order tests like a C-peptide test (which measures how much insulin the body is still producing) and an autoantibody panel (which checks for markers that indicate an autoimmune attack on insulin-producing cells). These tests help distinguish between the two types of diabetes, especially in cases of rapid onset or adults diagnosed with type 1 diabetes.
We ran the tests and confirmed. I was diagnosed with type 1 diabetes as an adult at the age of 42.
Why This Specialist Doctor Visit Was So Different
Another reason this visit felt so much different is that it seemed much more proactive than reactive. During the appointment when I was first diagnosed with diabetes it felt like my entire world was crashing down because of the urgency (or my perceived urgency) based on the deluge of information I was being given and the way it was being given.
I thought that the changes to my daily life would be cataclysmic and that I would have to constantly carry bulky diabetic supplies, medications, insulin, syringes, test kits and strips, and so on. I thought my travel life was definitely being hijacked and that enjoying international cuisines was definitely no longer going to be an option. In hindsight, that was mostly based on my own ignorance of diabetes and diabetes care in general.
Week 2 – My Life—Nor Travel Life—Wasn’t Over
My diabetes specialist sat with me for almost an hour and slowly dispelled so many myths, unwarranted assumptions, and negative stigmas that I had somehow “acquired” over the years. I’m fairly ashamed of that fact; that I had allowed myself to be so ignorant about a disease that more than 1/3 of American citizens will deal with. Yes, nearly 35 million Americans have diabetes and nearly 90 million American adults have prediabetes, per the CDC.
The specialist let me know how far diabetic care had come in recent decades. Things like compact flex pens to take insulin—with many days worth of doses inside—corrected my misconception about carrying and curating masses of traditional needles. Continuous glucose meters have the ability to consistently track blood glucose levels without the need to Napoleonically bludgeon your digits multiple times a day.
Apps exist to help track every little detail of daily diabetic nuances and stats can automagically be sent to the physicians office so that treatment adjustments only require an email as opposed to an expensive office or virtual visit.
When I Left The Specialist’s Office…
I left that visit feeling much more hopeful about the reality of being diagnosed with diabetes and how it might be less invasive in my life than I originally thought. While still pretty darn invasive, mind you, but people with diabetes have so many more options than I originally though. I was feeling much more confident about things. Well, other than the fact that the specialist ordered more labs and said that I was likely to actually be diagnosed as a Type 1 diabetic as opposed to Type 2.
Week 3 – Resources For New Diabetics & Type 1 vs. Type 2 Diabetes
One of the other things that my new specialist did was let me know about some of the free programs and resources that I had at my disposal under their network. Minimally, there was a program where I could have multiple appointments with area-specific specialists. Those include a diabetes-specific dietician, a clinical pharmacist, and a registered nurse.
That meant that I could have multiple appointments to not only be educated but to also just ask all the questions I could come up with about being diagnosed with diabetes and how to proceed.
Immediately after leaving that appointment, I got calls from those people to set up appointments and within 3 days I was sitting with a dietician talking specifics about how my primarily vegetarian diet would need to be adjusted. A day later I was on a 1-hour phone conversation with a clinical pharmacist not only talking about the possible different medications, but how I was going to afford them. She helped me find programs for reduced-cost drugs as well as pharmacies that might have lower-cost prescriptions.
That last part—lowering the cost of diabetes care—might have been one of the biggest helps. Hearing things like the cost of diabetes care potentially being in the 5-figure range…per year…had recently gotten me feeling pretty helpless in the financial department.
Diagnosed With Type 1, Not With Type 2 Diabetes
One of the first things my specialist said was that it was likely to be diagnosed Type 1 diabetic just because of how high my A1C shot up. Also because of how quickly the onset and symptoms happened over the course of only a few weeks. More tests were ordered and it was shortly confirmed that I was now diagnosed Type 1.
But what does being diagnosed Type 1 vs. Type 2 really mean to the layperson? Here’s my extremely quick and truncated take on them. There’s much more to it, so I suggest you use this as a starting point and then go deep dive. I suggest later visiting the American Diabetes Association site for starters.
What Is Type 2 Diabetes?
Type 2 diabetes means the cells of the body that process glucose become insulin resistant, meaning they kind of don’t listen to the insulin anymore when it brings glucose along to be processed. Lifestyle is often a contributing factor to Type 2 diabetes. Things like being inactive or overweight can play heavily. But genetics may also be a contributing factor among other things.
What Is Type 1 Diabetes?
Type 1 diabetes is an auto-immune disease, which means you can kind of “catch” it, but it seems the experts don’t really know why, although that’s changing. Then your immune system turns into a real A-Hole and attacks and destroys the insulin-producing beta cells in the pancreas…which can’t be re-grown or re-produced as of this writing. After these beta cells are destroyed, the body is unable to produce insulin or as much insulin, as before.
Now, while some diabetes care is similar for both, the big difference with being diagnosed with type 1 diabetes is much more of a dependence on supplying and regulating insulin manually, since the body simply isn’t making as much or any insulin.
This leads to dealing with the complicated high and low blood glucose roller-coaster and the potential effects of hypoglycemia in the short term. This is by no means downplaying Type 2, but just noting that the more elevated “insulin-dependent” nature of being diagnosed with Type 1 seems to make it much high-maintenance and more volatile on the daily.
Hyperglycemia vs. Hypoglycemia
Having high blood sugar or glucose levels (hyperglycemia) for extended lengths of time (like weeks, months, or years) can cause nasty issues like diabetic kidney disease, End-Stage Renal Disease, nerve damage, diabetic retinopathy, and other loveliness that can affect the eyes, kidneys, nerves, and heart.
Low blood sugar or glucose levels (hypoglycemia) are an immediate threat. Essentially, the brain cannot function without proper amounts of glucose. So when levels drop well below normal, things like dizziness, headache, confusion, muscle weakness, seizures, unconsciousness, and potential coma or death start to come into play, among other things.
Again, I suggest visiting the American Diabetes Association site to get a true understanding.
Week 4 – Quiet Acceptance And Momentary Calm
During the first 3 weeks of being diagnosed with diabetes I racked up at least the following:
- 5 in-person and 2 virtual/phone doctor or support appointments
- 8+ new prescriptions for new medications, treatments, or diabetes gear—some redundant or eventually replaced after being diagnosed with Type 1 diabetes, since the treatments differ between 1 & 2
- 2 new glasses prescriptions, both of which became irrelevant eventually (don’t get me started…)
- 2 new diabetes cookbooks (One a gift from my sometimes roomie who was very patient with me during this time…)
- 3 hypoglycemic nighttime blood glucose lows between 42-60mg/dL, which had me waking up drenched in sweat, shaky, dizzy, and not thinking straight to say the least (One night almost talked myself into laying back down sleeping it off. WTF?!)
- Unknown new health debt/bills due to most of the above
To Say It Was Overwhelming Would Be An Understatement
Especially as a single person not in a relationship at the moment and without the foresight to take a friend with me to the early appointments. It was frustrating and lonely not to have someone to “assist” when my brain…or heart…was short-circuiting. It’s natural only to want to burden family or friends so much with your problems, so I was wary of that.
But about the time I went to my “last” appointment—for at least a couple of weeks at least—a friend offered that I housesit his beach house while their family was away. Either a couple of days or up to a couple of weeks, whatever I wanted or felt comfortable with. He knew I could use the time away and he would feel better with someone in the house, a potential win-win.
Initially I tried to talk myself out of it, thinking that staying in my relative shame spiral in my safe space was best for me. Maybe a path of least resistance?
Stop Overthinking Everything And Just. Say. Yes.
But then I listened to my own advice to “just say yes” when unique opportunities arise, and I took it. I mean, this was exactly why I worked hard to become a location-independent digital nomad. The reason I chose to be a penny-pinching, budget-traveling remote worker.
Even with my choice to go, I assumed that being completely isolated by myself at the beach would quickly drive me insane and that I would be “home” within days. But exactly the opposite happened.
Week 4 – The Calm After The Storm
I ended up housesitting and working next to the calming sound of the ocean for a full 10 days. I concentrated on learning how to and eating better. Also exercising almost every day among, another new dictate from the doctors. I spoke about being diagnosed with type 1 diabetes publicly for the first time, since I was ready to finally pull off the bandage.
Knowing I could use my websites or speak to educate and help others, whether they are diagnosed with diabetes or not, gave me more sense of purpose regarding my new changes.
Essentially I was able to finally start processing all that had happened and the unavoidable reality of what my future would look like. I slowed down and absorbed things. I got back to my normal working habits, no longer being controlled by the false “urgency” of figuring everything out right now.
Calming down and taking it slow and methodically was much more healthy in the moment, and giving myself some grace to be human and emotional or fallible was completely appropriate.
There’s a saying in the wilderness first responder community that often rings true:
“Seconds never matter, minutes rarely do.”
It means that when things are rushed, details are missed. Haste makes waste. That slower is often faster in the long run. This is a marathon, not a sprint…or any other cliche you want to insert here. They’re cliches for a reason my friend—there’s truth in them.
What Now?
Now that I’ve made it through the first month of craziness, I’m realizing that it’s going to take a long time to get in any rhythm. There’s so much to learn, and no two bodies react the same way to diabetes, food, medications, exercise, etc.
And while I’m regularly frustrated at my inability to regulate right now, I’m trying to remind myself that this is the long con. I’m trying to calm down and just keep taking more steps forward than backward in my education and practices. I suggest you do the same.
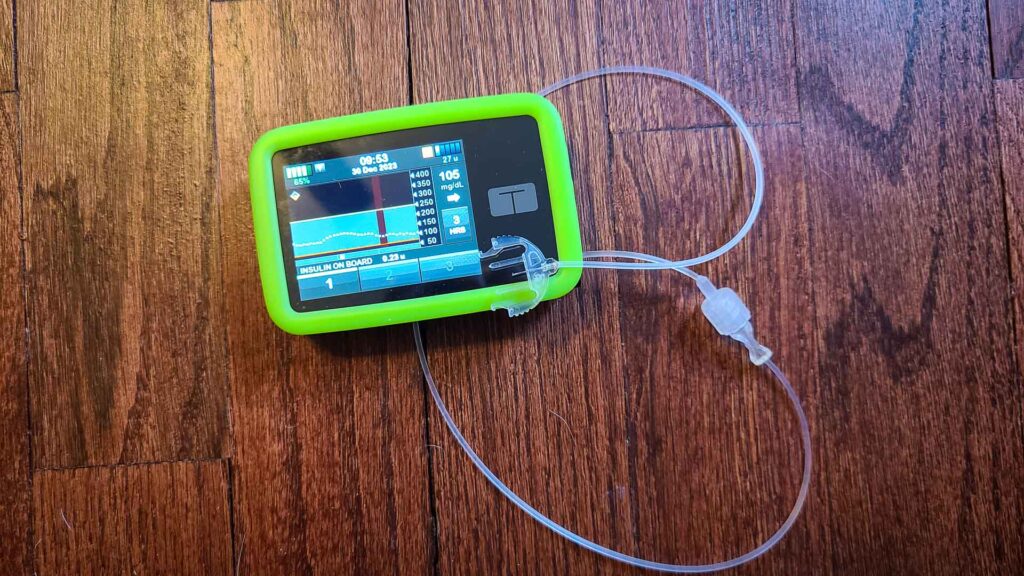
I’ll consider getting an insulin pump to help me take insulin, but I want to learn how to manage my blood sugar level manually, with insulin pens, for the moment. I’ve already had a few people with type 1 diabetes tell me using an insulin pump gives a much better quality of life for type 1 diabetics, but I’ll want to have a baseline with multiple daily injections first.
What Can You Do?
We all need to better understand what’s going on around us in an effort to be better humans and gain more empathy toward others. Please don’t be passive about diabetes, whether you have it or not, learn some more. Get your physical every year over age 30, and make sure they do the blood test they should—specifically a blood glucose A1C test.
Cheers!
—Jason







Jason, sorry to hear about the diabetes. I know how tough it can be but there is hope. My life partner (Jo Ann) has had Type 1 for several years and we have continued to have a full life traveling all over the globe. But I will admit we have had a few scary moments with hypoglycemic events, twice in Africa. Always carry glucose tablets or something for a quick jolt when needed.
Your write up is so spot on and what a great reference for others who may be learning they have diabetes. Thank you for sharing.
Wishing you all the best in 2021 and beyond.
Bob
Appreciate these words Bob! Yep, this is just another thing to learn and add to the travel toolbox. If life were boring it wouldn’t be memorable!
Cheers!